Abstract
Introduction:
Hematological malignancies are more and more common in elderly patients. Acute myeloid leukemia (AML) in elderly patients would have more unfavorable cytogenetics, frequently express drug resistance, respond less well to chemotherapy and more likely to be preceded by the myelodysplastic syndrome (MDS), while MDS is a predominantly malignant disease of elderly patients, with a median age of approximately 75 years old at diagnosis and more than 80% are noted to be older than 60 years. Although allogeneic hematopoietic stem cell transplantation (allo-HSCT) remains the curative therapy for refractory AML or high risk MDS, old age had been a limitation to access the eligibility for allo-HSCT and seldom prospective trial evaluates the outcomes for elderly patients with allo-HSCT. Here, we conducted a retrospective study to analyze the prognostic factors predicting outcome of elderly patients with allo-HSCT for acute leukemia and MDS at our institution during a 10-year period.
Method
We reviewed patients with diagnosis of acute leukemia or MDS, who underwent allo-HSCT at age older than 50 years old from January 2003 to December 2014. Clinical characteristics including age, sex, underlying disease, type of allogeneic transplant, conditioning regimens, European Group for Blood and Bone marrow Transplantation (EBMT) risk score, and presence of acute graft-versus-host disease (aGVHD) or chronic GVHD (cGVHD) were collected and analyzed. Cox proportional hazard model was adopted to explore the independent prognostic factors for overall survival (OS), disease-free survival (DFS) and non-relapse mortality (NRM).
Results
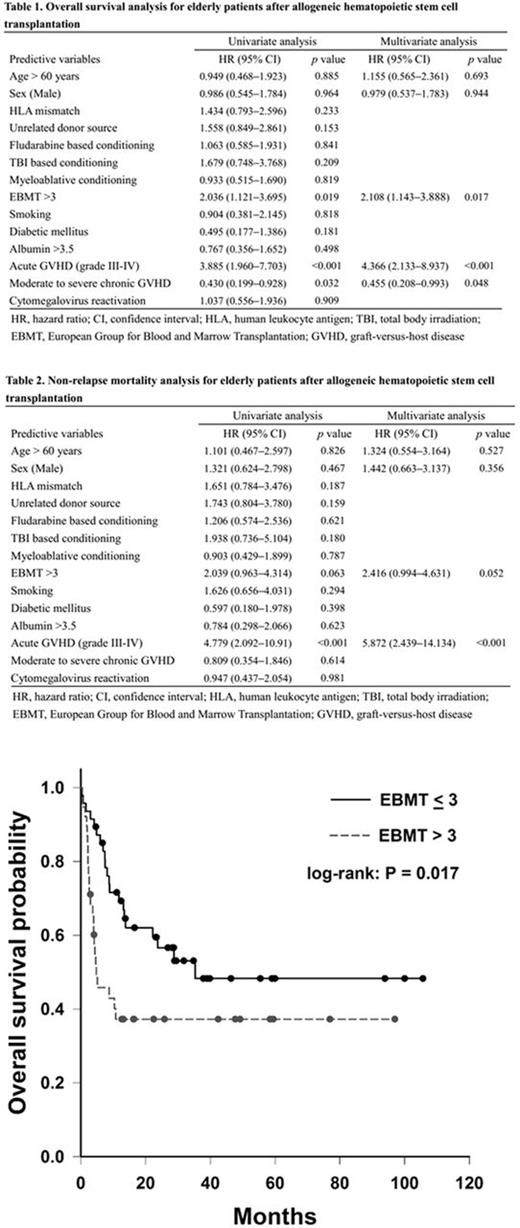
A total of 85 elderly patients were included during study period and the medial age at allo-HSCT was 55 years old. There were 63 (74%) patients receiving allo-HSCT for AML, which was the most common indication for transplantation in this cohort. 47 (55%) recipients' stem cell source were unrelated donors, while 46 (54%) patients underwent myeloablative conditioning regimens. 14 (17%) cases developed grade III-IV aGVHD, while 22 (26%) had moderate to severe cGVHD. The significant prognostic factors for worse OS after transplantation (Table 1) were EBMT risk score > 3 (hazard ratio [HR] 2.10, 95% confidence interval [CI] 1.14-13.88; P=0.01), and grade III-IV aGVHD (HR 4.36, 95% CI 2.13-9.93; P < 0.01), while patients with moderate to severe cGVHD would have better OS (HR 0.45, 95% CI 0.20-0.99; P=0.04). Similar finding was noted in DFS analysis: EBMT risk score > 3 (HR 2.27, 95% CI 1.31-3.94; P < 0.01), aGVHD (HR 4.70, 95% CI 2.41-9.17; P < 0.01), and moderate to severe cGVHD (HR 0.46, 95% CI 0.23-0.90; P = 0.02). In addition, EBMT risk score > 3 (HR 2.41, 95% CI 0.99-4.63; P = 0.05) and grade III-IV aGVHD (HR 5.87, 95% CI 2.43-14.13; P < 0.01) significantly correlated with non-relapse mortality (Table 2). The OS of patents with EBMT risk score < 3 was significant better than those with EBMT risk score >3 (log-rank p= 0.01), and Kaplan-Meier curve of OS divided by EBMT risk score were illustrated in figure 1.
Conclusion
We identify EBMT risk score > 3 and grade III-IV aGVHD as adversely prognostic factors for OS, DFS and NRM in elderly patients underwent allo-HSCT. Development of moderate to severe cGVHD allows elderly patients to have better OS as well as DFS, and interestingly, it would not increase NRM significantly. It indicates graft-versus-leukemia may be essential important in survival and disease control for elderly patients experiencing allo-HSCT. This cohort study suggests that EBMT risk score > 3 predicts poor outcomes and careful management of GVHD may lead to better survival for elderly patients experiencing allo-HSCT.
Key words: acute leukemia, myelodysplastic syndrome, elderly, allogeneic hematopoietic stem cell transplantation, European Group for Blood and Bone marrow Transplantation (EBMT) risk score, graft-versus-host disease
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal